Yes, smokers can get dental implants, but their success rates are significantly lower without proper intervention. However, with the right preparation, cessation strategies, and specialized care protocols, smokers may be able to achieve successful outcomes.
Continue reading to discover the specific challenges smokers face and the proven solutions that can dramatically improve implant success rates.
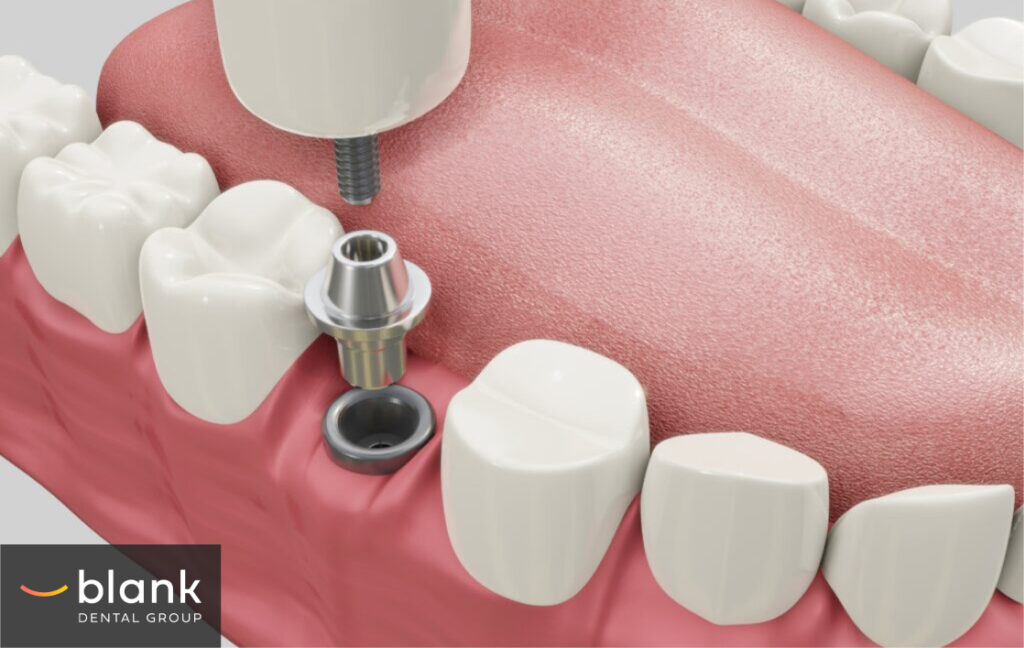
What Dental Implants Are and How They Work
Dental implants are titanium posts surgically embedded into the jawbone to replace tooth roots. They support replacement teeth that function like natural ones. A complete implant system includes the titanium implant, an abutment connector, and a custom-made crown that matches the surrounding teeth.
The Osseointegration Process
Osseointegration is the biological fusion between bone and implant that ensures stability. After placement, bone cells gradually grow onto the titanium surface, creating a direct structural connection.
This process begins with initial stability, followed by a brief decrease in weeks 2-4 as old bone remodels. Secondary stability develops between weeks 4-12 as new bone forms, with complete integration occurring within 3-6 months, resulting in a permanent bond.

Success Rates for Non-Smokers
Non-smokers experience excellent long-term outcomes with dental implants. The 5-year success rate reaches 95-98%, with 10-year rates of 93-97% and lifetime success around 90%. These impressive statistics result from better blood circulation, stronger immune response, higher bone density, healthier oral tissues, and the absence of tobacco chemicals that interfere with healing.
This combination of biological advantages and advanced implant technology makes implants the premier tooth replacement option for non-smoking patients.
The Impact of Smoking on Oral Health
Smoking introduces over 7,000 chemicals into the oral cavity, causing direct damage to gum tissues. Tobacco use restricts blood vessels and reduces oxygen supply, leading to chronic inflammation of the gums. Over time, this inflammation progresses to periodontitis, causing the gums to recede from teeth and creating pockets where bacteria thrive.Smoking also accelerates bone loss in the jaw. Nicotine inhibits osteoblast activity—cells responsible for bone formation—while stimulating osteoclasts that break down bone tissue. Studies show smokers experience up to 4.7 times more bone loss around teeth compared to non-smokers, creating a poor foundation for dental implants.
Reduced Blood Flow and Healing Capacity
The vasoconstrictive properties of nicotine significantly impair blood circulation to oral tissues. This reduced blood flow means fewer nutrients and oxygen reach the surgical site after implant placement. Consequently, smokers experience delayed healing times—often 2-3 times longer than non-smokers.
White blood cells, essential for fighting infection, are also compromised in their function and mobility, leaving smokers more vulnerable to post-operative infections. The body’s natural inflammatory response, crucial for initial healing, becomes dysregulated, further complicating recovery.

Chemical Interference with the Healing Process
Tobacco’s chemical compounds directly interfere with cellular processes critical to implant integration. Carbon monoxide from cigarette smoke reduces oxygen transport in the bloodstream, while hydrogen cyanide inhibits enzymes necessary for oxygen metabolism at the cellular level.
Nicotine and cotinine specifically disrupt fibroblast function—cells that produce collagen essential for tissue repair. Additionally, these chemicals impair the formation of new blood vessels (angiogenesis) that must develop around the implant.
The result is compromised wound healing at the molecular level, creating an environment where osseointegration becomes significantly more challenging.
Smoking is Directly Linked to Implant Failure
Research by the National Library of Medicine conclusively demonstrates that smoking significantly increases dental implant failure rates. A comprehensive meta-analysis of 292 publications examining 35,511 implants in smokers and 114,597 implants in non-smokers found that smokers have a 140.2% higher risk of implant failure.
Statistical evidence in the study shows implants in smokers had significantly higher failure risk compared to non-smokers. This failure risk was pronounced in both the maxilla and mandible. Additionally, marginal bone loss averaged 0.580 mm greater in smokers.
The biological mechanisms behind these statistics include tobacco’s vasoconstrictive effects, which reduce blood flow to healing tissues, and chemical interference with cellular repair processes. The compromised healing environment creates conditions where osseointegration is less likely to succeed, directly contributing to the higher failure rates observed in clinical studies.
These findings emphasize the importance of addressing smoking status before implant procedures, as the correlation between tobacco use and implant failure is strongly supported by statistical evidence.
Specific Challenges for Smokers
Smokers face significantly higher risks of peri-implantitis, with rates nearly triple those of non-smokers. This inflammatory condition affects tissues surrounding implants and leads to progressive bone loss that can ultimately cause implant failure. Tobacco chemicals weaken the immune response, creating an environment where bacteria more readily colonize implant surfaces.
Nicotine’s vasoconstrictive effects restrict blood flow to surgical sites, reducing oxygen and nutrient delivery that’s essential for tissue regeneration. This delayed recovery extends the healing period and often increases discomfort throughout the process.
Osseointegration is fundamentally compromised in smokers as tobacco toxins disrupt the balance between bone formation and resorption. This imbalance interferes with the critical fusion between implant and bone, which ensures stability. Research demonstrates that smokers achieve less bone-to-implant contact compared to non-smokers, directly impacting long-term success rates.
The risk of post-operative infections rises substantially in smokers due to tobacco’s immunosuppressive effects. Smoking impairs neutrophil function, reduces antibody production, and disrupts cytokine balance—all vital components of the body’s defense system. This creates vulnerable conditions where oral bacteria can infiltrate surgical sites, potentially requiring implant removal.

Solutions and Strategies
Smoking cessation protocols offer the most effective approach before implant surgery. Most dental practices recommend quitting at least two weeks prior to surgery and continuing abstinence throughout the healing period. Nicotine replacement therapies like patches or gum can help manage withdrawal symptoms while avoiding smoke exposure. Even a short cessation period can improve surgical outcomes significantly.
For patients unable to quit completely, temporary smoking reduction approaches can still provide benefits. Cutting consumption by at least half, especially in the 48 hours before and after surgery, helps minimize immediate surgical complications. Some practitioners recommend scheduling implant surgery early in the day to extend the natural overnight non-smoking period.
Understanding how to care for dental implants is especially critical for smokers. Enhanced hygiene practices are essential for smokers receiving implants. This includes more frequent professional cleanings (every 3 months versus the standard 6 months), chlorhexidine rinses twice daily, and specialized oral irrigators to clean implant sites. Water flossers with antimicrobial solutions provide additional protection against the elevated bacterial burden smokers typically experience.
Special aftercare considerations for smokers include extended healing periods, with many practitioners doubling the typical osseointegration timeline before placing final restorations. Bone grafting procedures are often required to address deficient bone density. More frequent follow-up appointments allow for early intervention if complications arise, and some clinics use advanced imaging techniques to monitor bone density changes around implants in smoking patients.
Smoke & Implant Success Without Compromise
While smokers face significant challenges with dental implants, proper protocols can substantially improve outcomes. With appropriate cessation strategies, enhanced hygiene practices, and specialized aftercare, smokers can still benefit from this life-changing dental treatment.
The key is a collaborative approach between the patient and dental professional, where both parties acknowledge the risks but work together toward the shared goal of successful, long-lasting implants.